Presentation & Cause
A pacemaker is any device that sends controlled electrical impulses to certain areas of the heart in order to stimulate cardiac contraction when the heart’s intrinsic electrical system is not functioning normally. The overall purpose of pacemakers is to restore normal electrical activity, improve heart function, and regulate cardiac pacing as part of cardiac resynchronization therapy (CRT).
Based on current guidelines, approximately 40% of patients with systolic heart failure are cardiac resynchronization therapy candidates. For patients with heart failure, myocardial dysfunction, and prolonged ventricular depolarization on a surface electrocardiogram (ECG), CRT has been proven effective.
Delivery methods for CRT include a pacemaker or a combined pacemaker-defibrillator. The most ideal CRT device type for specific populations with regard to patients’ longevity, quality of life, and cost of care is not clearly defined despite extensive research conducted over the past 2 decades.1
CRT: Diagnostic Workup & Differential Diagnosis
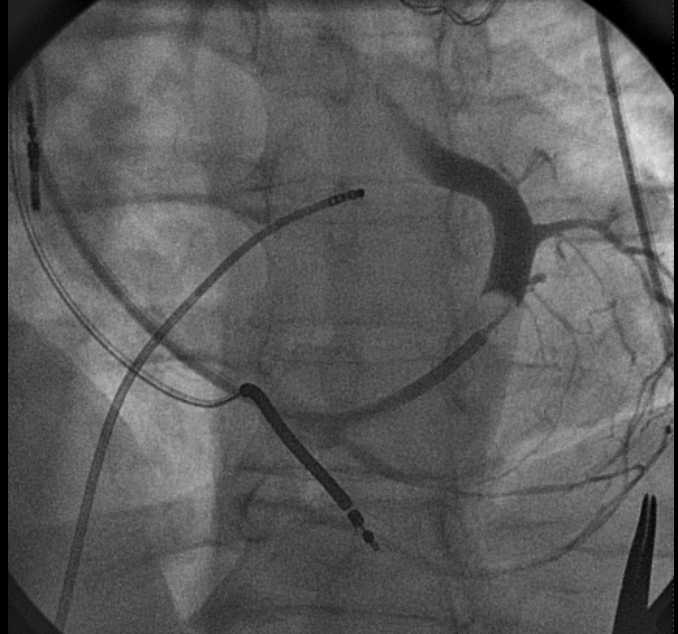
Pacemakers consist of a pulse generator, pacing leads or wires, and an electrode at the end of each lead to carry the electrical signals to the relevant area of the heart. The pulse generator is implanted under the skin, most commonly in the left anterior chest wall or the left axilla. The pacing leads are inserted into the relevant chambers of the heart.
Modern pacemakers rely on a computer that monitors the electrical activity and tailors the function of the pacemaker to the electrical activity that already exists in the heart. Pulse generators can also be utilized for implantable or external pacemakers as necessary.2
Most commonly used pacemakers are permanent, single, and dual chamber pacemakers. Common cardiac pacing indications for a permanent pacemaker are symptomatic sinus node dysfunction (sinus bradycardia or sinus pauses), third or type 2 second atrioventricular (AV) -block, and permanent atrial fibrillation with symptomatic bradycardia.
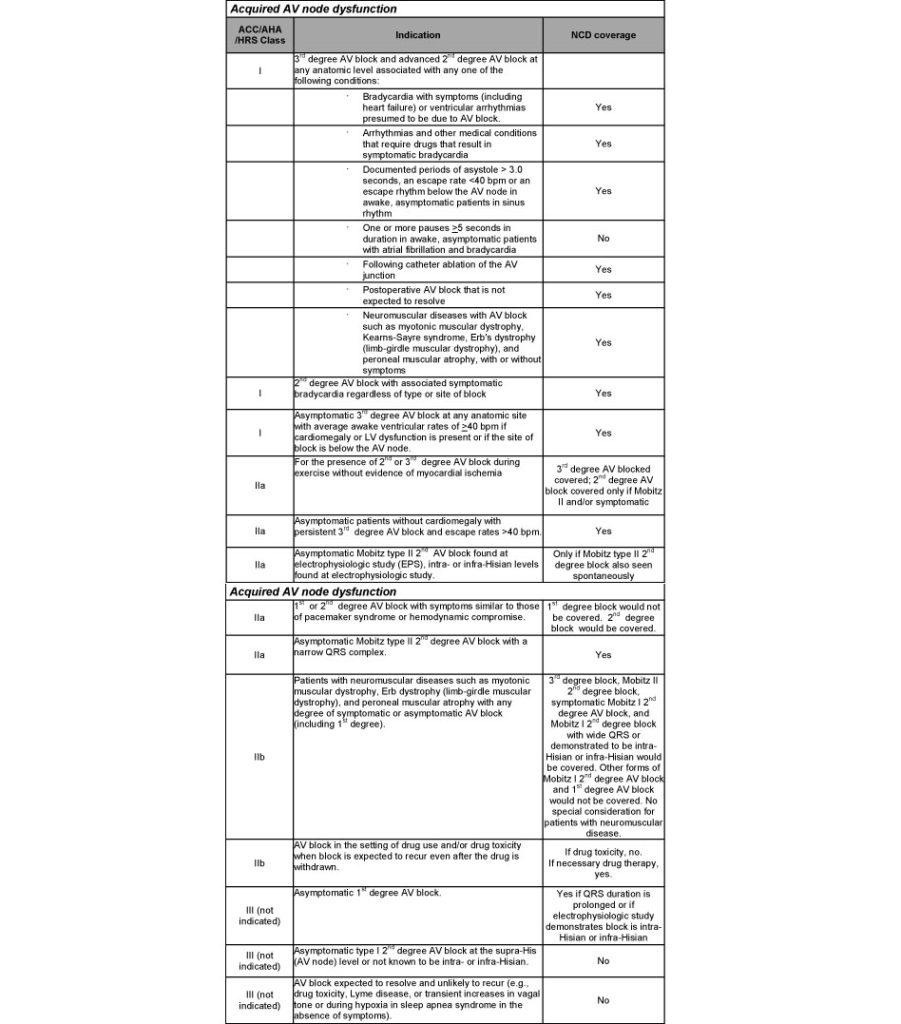
Symptomatic indicators that may be treated with a pacemaker include symptomatic chronotropic incompetence and symptomatic pronounced AV block. A common indication for the use of a pacemaker is severe heart failure.3
When a patient already has a pacemaker implanted, an ECG, which detects the heart’s rhythm and electrical activity, can be interpreted and then used to identify the type of pacemaker the patient currently has.
The pacemaker intervention on an ECG can be seen as a sharp vertical line on all the leads on the ECG as electricity is transferred to the heart. More specifically, a line before the P wave indicates that the lead has been inserted into the atria. Alternatively, a line before the QRS complex (Q wave, R wave, and S wave) indicates that the lead is in the ventricles.4
CRT Device Overview & Selection Options
There are several different ways in which pacemakers can be categorized and chosen for a particular patient. They are often referred to by the number of the heart’s chambers they can pace.
- A single chamber pacemaker can either pace the right atrium or the right ventricle. The lead is placed in the right atrium if the AV conduction in the heart is normal and the issue is with the sinoatrial node. This stimulates depolarization in the right atrium, and then the electrical activity passes to the left atrium, through the AV node, and to the ventricles, promoting normal contraction of the heart. If the AV conduction in the patient is abnormal, the physician may place a single chamber pacemaker in the right ventricle, allowing it to bypass the atrium and stimulate the ventricular contraction directly.1
- A dual chamber pacemaker can pace both the right atrium and the right ventricle. By doing so, it can synchronize the contractions of the atria and the ventricles.1
- A biventricular pacemaker can pace the right atrium, right ventricle, and left ventricle. The use of a biventricular pacemaker is indicated by ventricular dyssynchrony, which can occur from either right ventricular pacing and/or from underlying cardiomyopathy. This pacemaker synchronizes the contractions of all the chambers, optimizing overall heart function. A common indication for the use of a biventricular pacemaker to conduct cardiac resynchronization therapy is severe heart failure.3
Pacemakers are also categorized based on their duration. There are permanent pacemakers that contain a battery that typically lasts for 5 to 10 years, after which the generator needs to be replaced. While cardiac pacing is most commonly accomplished using a permanent pacemaker, temporary pacing can be lifesaving in critical care patients with severe symptoms and acute instability.5 Temporary pacemakers remain implanted for several days or a week and can establish normal sinus rhythm in cases of bradyarrhythmias, tachyarrhythmias, and heart block.5
- Transvenous pacemakers are those from which the wires are implanted into the internal jugular vein, yet the power source and circuitry remain external.6
- Transcutaneous pacemakers conduct an electrical current applied to the patient’s skin. A transcutaneous pacemaker is only used during bradycardic arrests in order to buy the necessary time to place a transvenous pacemaker.6
- Epicardial pacemakers are occasionally placed at the time of cardiac surgery.6 Contrary to conventional pacemakers, temporary epicardial pacing wires are almost always implanted at the conclusion of cardiac surgery to treat bradydysrhythmias, particularly AV block, or to control heart rate.2
Pacemakers can also be categorized by whether they have the ability to defibrillate the heart in the event of ventricular fibrillation (VF) or sustained ventricular tachycardia (VT). This ability would classify those pacemakers as implantable cardioverter defibrillators (ICD).7
ICDs are used to terminate VT and VF in high-risk patients. ICDs have both typical pacing/sensing electrodes and 1 to 2 defibrillation electrodes composed of coils and wire. The metal housing of the generator itself can serve as a third electrode. These defibrillators continually monitor the heart and, in the case of a patient having a shockable arrhythmia, an ICD shocks the heart in order to return the heart rate to proper rhythm.
The first indication is secondary prevention of cardiac arrest or sustained VT in the absence of a completely reversible cause. The second indication is the primary prevention of sudden cardiac death.7
Patient & Special Populations Consideration
Regardless of cardiac pacing indication, reversible ideologies of the conduction disease must be ruled out first before placing the device. Reversible ideologies can include medications, infection, electrolyte disturbances, and ongoing ischemia. For patients who require a rhythm control strategy, cardioversion is a vital option for atrial flutter and atrial fibrillation management through synchronized direct current, electrical shock, or application of antiarrhythmic drugs.8
Cardioversion is a medical procedure that replaces an irregular heart rhythm with brief, low-energy shocks. In the emergency room, patients can be cardioverted quickly to treat their immediate symptoms and enable discharge. This eliminates the need for anticoagulation in low-risk patients as well as the requirement for heart-rate control prescriptions.9
Electrical cardioversion is the best treatment option for severely hemodynamically compromised patients with new-onset atrial fibrillation or atrial flutter because it stops atrial fibrillation in over 90% of cases.8
Monitoring Cardiac Pacers
Because permanent and temporary cardiac pacers expire over a certain period of time and can have dangerous complications, they require constant monitoring. Implantation-related complications that could arise from the use of a pacemaker include pocket hematoma, pocket infection, pneumothorax, hemothorax, lead dislodgement, and, rarely, a cardiac perforation/tamponade.
Many complications could also be delayed, giving even more reason to continue monitoring the patient. These delayed complications include a lead fracture, insulation break, infection (pocket or lead), thrombosis/stenosis of veins, pacing-induced cardiomyopathy, pacemaker syndrome, and pacemaker-mediated tachycardia.10
References
1. Canterbury A, Saba S. Cardiac resynchronization therapy using a pacemaker or a defibrillator: Patient selection and evidence to support it. Prog Cardiovasc Dis. 2021;66:46-52. doi:10.1016/j.pcad.2021.04.003
2. Cronin B, Dalia A, Goh R, Essandoh M, O’Brien EO. Temporary epicardial pacing after cardiac surgery. J Cardiothorac Vasc Anesth. 2022. doi:10.1053/j.jvca.2022.08.017
3. Glikson M, Nielsen JC, Kronborg MB, et al. 2021 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. Europace. 2022;24(1):71-164. doi:10.1093/europace/euab232
4. Prutkin JM. ECG tutorial: Pacemakers. UpToDate. Updated April 13, 2021. Accessed September 15, 2022.
5. Gammage MD. Temporary cardiac pacing. Heart. 2000;83(6):715-720. doi:10.1136/heart.83.6.715
6. Cunningham MA, Ferrara E. Temporary Cardiac Pacing. In: L’Ecuyer KM, Young E, eds. Cardiac Vascular Nurse Certification Review. Springer Publishing Company, LLC; 2022:179-192.
7. Ellenbogen KA, Kaszala K. Cardiac Pacing and ICDs. 7th ed. Hoboken, NJ: John Wiley & Sons Ltd; 2020.
8. Brandes A, Crijns HJGM, Rienstra M, et al. Cardioversion of atrial fibrillation and atrial flutter revisited: current evidence and practical guidance for a common procedure. Europace. 2020;22(8):1149-1161. doi:10.1093/europace/euaa057
9. Stiell IG, Sivilotti MLA, Taljaard M, et al. Electrical versus pharmacological cardioversion for emergency department patients with acute atrial fibrillation (RAFF2): a partial factorial randomised trial. Lancet. 2020;395(10221):339-349. doi:10.1016/S0140-6736(19)32994-0
10. Asirvatham SJ, Friedman PA, Hayes DL. Cardiac Pacing, Defibrillation and Resynchronization: A Clinical Approach. 4th ed. Hoboken, NJ: John Wiley & Sons Ltd; 2021.
Sydney Murphy is the Associate Editor of HealthDay Physicians Briefing and a freelance science writer based in New York City. You can follow her on Twitter @SydneyLiz_Murph.