AFIB Causes & Presentation
A common type of cardiac arrhythmia, atrial fibrillation (AFib) is considered a tachyarrhythmia.1 In the United States, there are more than 454,000 hospitalizations with atrial fibrillation listed as the primary diagnosis each year, and atrial fibrillation contributes to about 158,000 deaths each year.2 Moreover, the number of people with atrial fibrillation and needing AFIB treatment is expected to double or triple by 2050.3
With atrial fibrillation, the atria do not contract in a strong, regular pattern.1 During this disorganized atrial activity, the heart may not pump enough oxygen-rich blood to the body. These arrhythmias can be classified as paroxysmal, persistent, permanent, or long-standing.3
People with atrial fibrillation are five times more likely to have a stroke than people without this arrhythmia. Risk of heart failure is also elevated with atrial fibrillation due to the gradual weakening of the heart muscle.1
Atrial fibrillation does not always present with symptoms, but when symptoms occur, they may include:3
- Fast heartbeat
- Irregular heartbeat
- Heart palpitations
- Lightheadedness
- Chest pain or pressure
- Nausea
- Dizziness
- Diaphoresis
- Fatigue
- Lower extremity swelling
- Dyspnea on exertion
- Shortness of breath
Atrial Fibrillation Risk Factors
Atrial fibrillation risk factors may include:3
- Older age (prevalence of approximately 1% in general population worldwide compared to 22% in individuals aged 80 and older)
- Hypertension
- Underlying congenital valvular, structural, or ischemic heart disease
- Underlying lung disease
- Obstructive sleep apnea
- Obesity hypoventilation syndrome
- Smoking
- Illicit drug use
- History of rheumatic fever
- History of pericarditis
- Hyperlipidemia
- Hyperthyroidism
Atrial Fibrillation Quick Facts – Infographic Embed
<a href="https://www.thecardiologyadvisor.com/ddi/atrial-fibrillation-management/"><img style="width:100%;" src="https://www.thecardiologyadvisor.com/wp-content/uploads/sites/17/2023/01/AFIB-Management-510x1280.jpg"></a><br>Infographic by: Cardiology Advisor <a href="https://www.thecardiologyadvisor.com/ddi/atrial-fibrillation-management/">Cardiology Advisor - Atrial Fibrillation</a>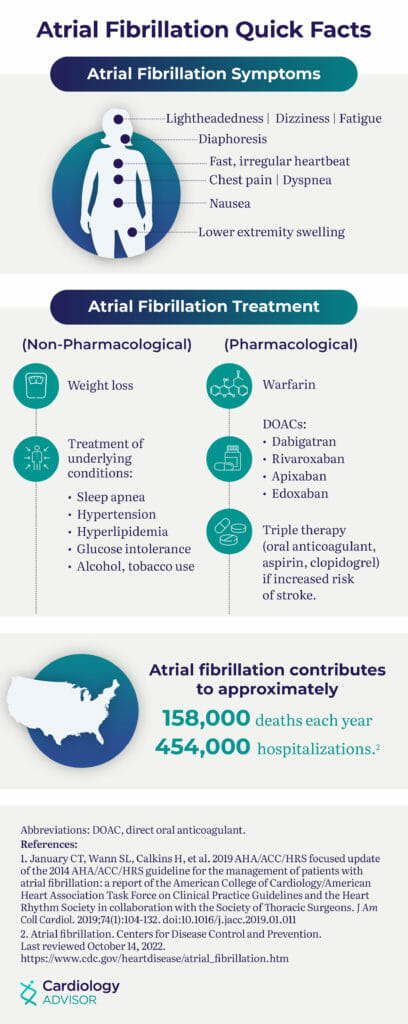
Atrial Fibrillation Differential Diagnosis & Diagnostic Workup
Patients with atrial fibrillation may present with mild or no symptoms or severe manifestations including heart failure or stroke.
Evaluating a patient for atrial fibrillation starts with taking a thorough history to uncover any potential risk factors and conducting a physical exam focusing on symptoms such as palpitations, chest pain, and shortness of breath.3 Moreover, extremities may be swollen and there may also be decreased pulses in both upper and lower extremities and integumentary signs of peripheral vascular disease including hair loss and skin breakdown.3
Healthcare providers should ask about symptom onset, duration of symptoms, and any aggravating factors leading up to symptoms.3 Also inquire about recent illnesses and the use of new medications, supplements, illicit drugs, or alcohol.
Patients may present with an irregularly irregular pulse. Heart rate usually ranges from 110 to 140/min.3 Still, this should be confirmed with electrocardiography.
Note that a normal test result does not completely rule out atrial fibrillation because electrocardiography may not capture a paroxysmal arrhythmia. For these reasons, a Holter or cardiac event monitor may be required to make an AFIB diagnosis.3, 4
Look for potential underlying causes of atrial fibrillation during the physical exam.3 For example, listening to the neck may uncover signs of carotid artery or thyroid disease, pulmonary examination may show signs of heart failure such as rales or wheeze, and a cardiovascular exam consisting of careful auscultation can spot underlying valvular pathology.
In addition, an abdominal exam to look for an enlarged liver and/or distention may indicate heart failure. It is important to evaluate the central and peripheral nervous system for signs of transient ischemic attack or cerebrovascular accident.
Diagnostic tests should include blood pressure measurement, electrocardiogram (ECG), and laboratory work.3 Note that on the ECG, atrial fibrillation presents with a narrow complex “irregularly irregular” pattern and no distinguishable p-waves. Fibrillary waves may or may not be present, and ventricular rate typically ranges between 80 to 180 beats/min.
Laboratory testing may include:3
- Complete blood count (CBC) for infection or anemia
- Basic metabolic panel for electrolyte abnormalities
- Thyroid function tests for hyperthyroidism
- Cardiac biomarkers and B-type natriuretic peptide (BNP) to rule out underlying cardiac disorder
- Liver and kidney function tests
- Drug screening, if indicated
- Sleep study, if sleep apnea is suspected
Imaging tests for atrial fibrillation should include a chest X-ray to screen for lung disease, and an echocardiogram to identify any other heart-related problems.
Additional testing may be necessary depending on the patient’s history, including a stress echocardiography and cardiac catheterization for ischemia or coronary artery disease.3
Potential differential diagnoses include atrial flutter, atrial tachycardia, multifocal atrial tachycardia, Wolff Parkinson White syndrome, and atrioventricular nodal reentry tachycardia.3
AFIB Management
Atrial fibrillation management guidelines call for rhythm control, rate control, and prevention of thromboembolism.3 Additionally, it is important to manage risk factors for stroke, prevent other heart rhythm problems, and heart failure.
If the cause of the atrial fibrillation is identified during the diagnostic process, AFIB treatment can target the cause. For example, if atrial fibrillation is a result of underlying thyroid disease, AFIB treatment can involve treating the thyroid disease to correct the atrial fibrillation.
Stroke Prevention in Atrial Fibrillation & AFIB Treatment
Stroke prevention typically entails the use of blood-thinning drugs, namely warfarin, direct-acting oral anticoagulants (dabigatran, apixaban, rivaroxaban, or edoxaban), and aspirin (recommended only in rare cases).3
About 60% of strokes that occur after an atrial fibrillation diagnosis can be prevented with anticoagulants.3
Use the point-based CHA2DS2-VASc score to assess stroke risk in all atrial fibrillation patients:3
- Congestive heart failure
- Hypertension
- Age (75 or older; assigned double points)
- Diabetes
- Stroke (prior episode; assigned double points)
- Vascular disease (prior heart attack, peripheral artery disease or aortic plaque)
- Age 65-74
- Sex (female)
Each risk factor gets a certain number of points from 1 to 2.
People with atrial fibrillation and elevated CHA2DS2-VASc score of 2 or higher should receive oral anticoagulation. Non-vitamin K oral anticoagulants, including apixaban, dabigatran, edoxaban, and rivaroxaban, are recommended over warfarin in most cases.
Always assess renal and liver function before initiating non-vitamin K oral anticoagulants.3 Other medications to help control the heart rate during atrial fibrillation include beta blockers, certain calcium channel blockers, and digoxin.
Additionally, beta blockers or antiarrhythmics can restore normal heart rhythm in atrial fibrillation. In cases of paroxysmal atrial fibrillation, for example, heart rate can be reset with medications or cardioversion.5
Lifestyle modifications also play a role in AFIB treatment and preventing stroke or other downstream consequences.
Patients with atrial fibrillation should be advised to:1-3
- Get regular physical activity
- Eat a heart-healthy diet
- Manage hypertension
- Avoid excessive alcohol and caffeine consumption
- Quit smoking or never start
- Control cholesterol
- Maintain a healthy weight
Nonpharmacotherapy for atrial fibrillation can be divided into two categories: surgical or nonsurgical. Procedures to stop or control the electrical impulses causing the arrhythmia include electrical cardioversion or catheter ablation, pacemaker, or other surgery.3 Pacemaker use is typically reserved for severe cases that led to heart failure.
Electrical cardioversion can “reset” the heart to a normal rhythm, but for some atrial fibrillation patients the arrhythmia may return.3 In these cases, antiarrhythmic medications are needed indefinitely to keep the heart’s rhythm and rate in the optimal range and help prevent irreversible structural and electrical remodeling that can occur with longstanding, persistent AF. It is important to note that a transesophageal echocardiogram should always be done prior to cardioversion in these patients to minimize the risk of stroke.3
Ablation is used when cardiac arrhythmias are not responding to long-term medications or electrical cardioversion.5 Types of ablation include pulmonary vein isolation ablation and AV node ablation with pacemakers. During pulmonary vein isolation ablation, radiofrequency (RF) or lasers are used in the pulmonary veins to block the abnormal electrical impulses.
During ablation of the AV node, catheters are guided to the heart where radiofrequency energy severs or injures the AV node. Device therapy is also an option. In these cases, an implantable atrial defibrillator can be used to treat symptoms and keep heart rhythm in check as part of AFIB treatment.6
Monitoring AFIB Treatment
Blood-thinning drugs can increase risk of bleeding. Patients on warfarin must take a monthly blood test to monitor their blood levels of international normalized ratio (INR).7 Patients should be told to call right away if they experience any unusual bleeding or bruising. The newer oral anticoagulants do not require monthly blood testing.8 Care must be taken for perioperative management in patients with atrial fibrillation who use a direct oral anticoagulant and are undergoing surgery to reduce risk of bleeding and stroke.
Monitoring can be continuous with implantable pacemakers, implantable cardioverter defibrillators or subcutaneous implantable cardiac monitors or only when symptoms occur.6
AFIB ICD 10 Codes
Here are several relevant ICD 10 codes for atrial fibrillation:
| I48.0 | Paroxysmal atrial fibrillation |
| I48.1 | Persistent atrial fibrillation |
| I48.2 | Chronic atrial fibrillation |
| I48.91 | Unspecified atrial fibrillation |
References
1. FAQ about afib. American Heart Association. Published 2021. Accessed August 24, 2022.
2. Atrial fibrillation. Centers for Disease Control and Prevention. Updated July 12, 2022. Accessed August 24, 2022.
3. Nesheiwat N, Goyal A, Jagtap M. Atrial fibrillation. In: Stat Pearls. NCBI Bookshelf version. StatPearls Publishing: 2022. Accessed August 24, 2022.
4. Diagnosis: Atrial fibrillation. National Health Service. Updated May 17, 2021. Accessed Aug. 24, 2022.
5. Non-surgical procedures for atrial fibrillation (AFib or AF). American Heart Association. Last reviewed July 31, 2016. Accessed August 24, 2022.
6. Devices for arrhythmia. American Heart Association. Last reviewed September 30, 2016. Accessed August 24, 2022.
7. A patient’s guide to taking warfarin. American Heart Association. Last reviewed September 30, 2016. Accessed August 24, 2022.
8. Atrial fibrillation medications. American Heart Association. Accessed August 24, 2022.
Denise Mann, MS, is a veteran freelance health writer in New York. Her work has appeared on HealthDay, among other outlets. She was awarded the 2004 and 2011 journalistic Achievement Awards from the American Society for Aesthetic Plastic Surgery. She was also named the 2011 National Newsmaker of the Year by the Community Anti-Drug Coalitions of America.
She has also been awarded the Arthritis Foundation’s Northeast Region Prize for Online Journalism, the Excellence in Women’s Health Research Journalism Award, the Gold Award for Best Service Journalism from the Magazine Association of the Southeast, a Bronze Award from The American Society of Healthcare Publication Editors, and an honorable mention in the International Osteoporosis Foundation Journalism Awards.
She was part of the writing team awarded a 2008 Sigma Delta Chi award for her part in a WebMD series on autism. Mann has a graduate degree from the Medill School of Journalism at Northwestern University in Evanston, Ill.
Updated: 03/29/2023